
CONGRATULATIONS, YOU’RE PREGNANT! ????
What’s Next on This Journey?
Whew… you did it! Maybe for you it was super easy and this is your 1st, 2nd or 3rd baby. Or maybe you’ve been through one heck of a fertility journey with lots of ups & downs & disappointments and FINALLY had success. Or maybe you weren’t even trying and yet here you are. You’re pregnant!
The changes that your body, mind and soul will experience over the next 40-43 weeks will blow your mind. It will be exciting, scary, confusing, joyous, exhilarating, fatiguing, interesting and one heck of a learning experience. All preparing you for the next big journey: MOTHERHOOD!
Even if this is not your first, your experience with each pregnancy will bring something new to the table. No two pregnancies are exactly alike.
Alright, let’s first start at the beginning. Oh, Wait! Exactly where IS the beginning of your pregnancy? We all know that it starts with “sperm meeting egg” but WHEN did this all happen?
Even though pregnancy is commonly said to last about 40 weeks (41 in France!), the timeframe is calculated from the first day of YOUR LAST MENSTRUAL CYCLE (LMP), NOT FROM THE MOMENT OF CONCEPTION! So even though you and your partner did the wild thing on vacay in the Bahama’s your pregnancy is calculated by counting from the 1st day of your last menstrual bleed.
The reason for using the last menstrual cycle as a starting point is its clarity and memorability. It’s easier to identify and track than the exact moment of ovulation or fertilization. When a woman ovulates or when the couple has sex culminating in sperm having a wild date with your egg, can very greatly… so we simply use when your last cycle occurred and count from that first day of the cycle. Most people think of pregnancy as lasting 9 months, but technically you can see that it’s closer to 10 because the 40-week count includes about a 2 week time period when you’re not actually pregnant. So you’ll be “pregnant” for close to 280 days from your last menstrual period.
Yeah, I know… it’s a little confusing. But this method gives us a standard to use with ALL women and a practical framework that helps healthcare providers and you to manage the pregnancy with consistency.
TRIMESTERS
Next you need to know that pregnancy is broken down into TRIMESTER (3 time periods) each last 3 months. We will dive into each of these trimesters a bit more deeply later but for now…. Each woman will experience some level of these symptoms in each trimester:
The FIRST TRIMESTER (1-12 weeks) may bring symptoms of nausea, emotional swings, fatigue, boobs full and a bit painful and increased urination.
The SECOND TRIMESTER (13-26 weeks) tends to be a period when many women feel a surge of energy, the “pregnancy glow” might show up, and symptoms from the first trimester start subsiding.
The THIRD TRIMESTER (27-40 weeks) comes with a number of challenges: back pain, fatigue comes back, asthma, frequent urination, and gas.
BODILY CHANGES
Your body will go through a large number of changes. Think of it this way… you’re getting ready to have someone move into your body and grow which will cause your body to have to “rearrange the furniture” every week (organs moving)!
Not only are your organs moving around and new ones being brought in… your HORMONES will have a few surges as the placenta and baby grow.
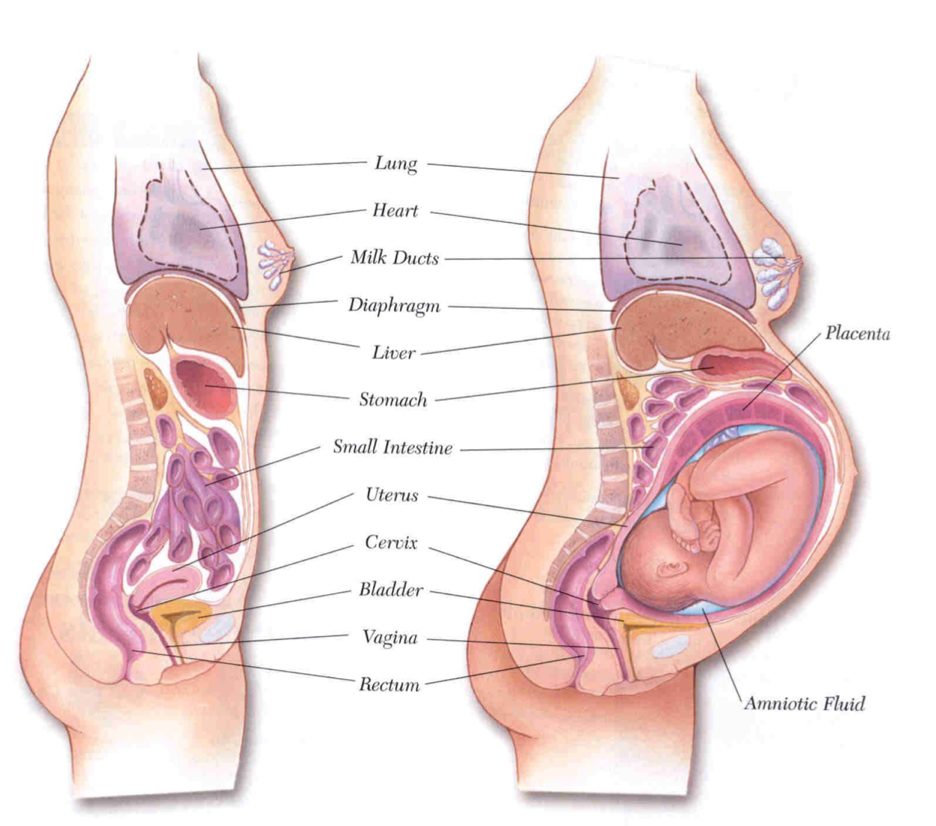
The placenta is an organ that develops in the first 4 weeks in the womb, also called the uterus, during pregnancy. The placenta is connected to a developing baby by a tubelike structure called the umbilical cord. Through the umbilical cord, the placenta provides oxygen and nutrients to your developing baby.
The placenta is crucial … it acts as a conduit for nutrients and oxygen from the mother to the baby which allows for proper fetal growth and development. It also helps to remove waste products from the fetus’s blood which protects the baby from infections, and it produces hormones that support the full term of the pregnancy. It’s not just a bridge between you and the baby… it also produces hormones and different molecules which you BOTH will need. Some of these molecules encourage new blood vessels to form to carry oxygen to the baby. Some help your body prepare to make milk and some boost your metabolism to supply energy.
These hormones (chemical messengers) are estrogens and progesterone that help maintain the uterine lining and regulate the mother’s own physiological changes throughout the pregnancy.
As I stated, your body makes new blood vessels along with more red blood cells. Hormones like progesterone, and possibly prolactin, help increase the production of these cells. Because of this, the pregnant woman needs 500mg more iron than normal! It’s super important to monitor your iron and ferritin blood levels in each trimester. This is a simple blood draw that any doctor can order for you. Don’t self diagnose that you need to supplement iron without proper guidance and testing.
You might notice some changes to your blood pressure during pregnancy. It’s not unusual to see a drop in pressure due to all the changes in hormones and blood volume. During the first trimester, many women will notice a slight decrease in blood pressure. This is due to the progesterone hormone surging. When blood vessels relax and widen this leads to lower pressure for mom. It’s a good thing… as this helps to ensure an adequate supply of blood to the growing fetus.
During the second trimester blood pressure usually remain stable. As the pregnancy progresses into the third trimester, blood pressure gradually starts to rise again, closer to pre-pregnancy levels.
Bottom line?
We now know that pregnancy vastly transforms the female body – affecting the blood, organs and immune system on a weekly basis.
A very comprehensive study encompassing 300,000 pregnancies with more than 160,000 women was completed in Israel. They followed women from conception up to 18 months after delivery and mapped out 76 blood markers and organ functions.
Notably, the scientists found that while 36 of the markers, including those related to blood clotting, bounced back within a month after delivery, 31 markers took more than 10 weeks to recover. For instance, some changes to the liver and immune system took around five months to return to pre-pregnancy levels, and several kidney markers took roughly half a year. Some bone and muscle markers took even longer. What exactly this means for women’s health is unclear, but it should be explored in future work, says Alon.
What’s more, a few other markers never returned to baseline levels, even over a year after birth. “The slightly old-fashioned view that by six or eight weeks after pregnancy, everyone’s completely back to normal, is clearly wrong,” says Lees.
For instance, iron levels remained low long after giving birth. Women are quite likely to be anaemic [have low iron levels] after delivery because of haemorrhaging and because a developing fetus takes a lot of the iron stores out of their bodies. We typically think it takes six to 12 months for iron stores to get back to normal – this study suggests it might take even longer.
Meanwhile, levels of a protein called CRP stayed high. CRP is affected by a number of different processes, certainly inflammation is one of them, but things like hormonal changes can also affect this. In another analysis, the team looked at markers in women who had preeclampsia – a condition during pregnancy where high blood pressure can cause headaches, vision problems and pre-term birth, and lead to fatal complications for both mother and baby if left untreated. This revealed that, before conception, women who developed preeclampsia had elevated levels of blood cell fragments called platelets and a protein called ALT compared with those who did not develop the condition.
For decades, the idea has been that the placenta doesn’t implant properly, and if it doesn’t implant properly, the blood supply is disrupted, it releases hormones and substances that lead to the mother getting high blood pressure. But some studies suggest that those who develop it have a different cardiovascular function before pregnancy – these findings add weight to this theory.
If further studies show that these pre-conception markers really do indicate the risk of preeclampsia, they could potentially be used to pinpoint women at high risk. Then you could target them with ways of improving health prior to pregnancy – either through exercise and lifestyle advice – to lower their risk. (Science Advances DOI: 10.1126/sciadv.adr7922)
HORMONE CHANGES
Whew! It can get quite wild, especially in the first trimester. Let’s take a look at each hormone change…
Pregnancy introduces a complex interplay of hormonal changes that have significant effects on a woman’s body, influencing everything from metabolism and fluid retention. These changes can affect your nutritional needs, energy levels, exercise capacity, and overall wellbeing.
THYROID HORMONE
Pregnancy causes the body to need more thyroid hormones so that the thyroid must make up to 50% more of these hormones. These levels play a crucial role during pregnancy, impacting both maternal health and fetal development. (Singh S, Haq N, Sandhu S. Thyroid Disease and Pregnancy. [Updated 2025 Jan 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538485/)
The significance of maintaining appropriate thyroid levels during pregnancy includes fetal development. Thyroid hormones are vital for the normal development of the baby’s brain and its nervous system. During the first trimester, the fetus depends entirely on the mother’s supply of thyroid hormones, which are transferred through the placenta. Insufficient thyroid hormone levels during early pregnancy can lead to developmental issues and lower IQ in children. Imbalances or low levels in Free T3 and Free T4 can lead to miscarriage and other complications.
It also impacts maternal health. Proper thyroid function in the mother is essential to maintain her health during pregnancy. Abnormal levels can lead to complications such as increased risk of miscarriage, preterm birth, preeclampsia, and placental abnormalities.
(There’s a lot to learn about thyroid optimization if you’re currently taking a thyroid hormone. Please ensure you read our THYROID TESTING article for a full explanation)
If you’re on a thyroid medication or glandular it’s not unusual to need an increase while pregnant or nursing. Work with a natural practitioner who thoroughly understand how to get and keep you at optimal levels (which are NOT usually the lab reported levels). If you have an autoimmune issue with your thyroid please read our article on HASHIMOTO’S Thyroiditis for full protocol details.
I cannot stress enough the importance of optimizing your thyroid function both in order to conceive as well as to maintain a healthy pregnancy. Please don’t just rely on your doctor telling you that your thyroid levels are fine without a second opinion from a practitioner who knows and understands how to work correctly with desiccated thyroid hormones or synthetics (levothyroxine or Synthroid).
Iodine supplementation is vital to support your thyroid no matter if you are or are not on thyroid hormones.
Should iodine be used for infertility?
The element iodine is an essential nutrient utilized by the thyroid glands, and deficiency of this element has been linked to reproductive failures. Iodide transporters are also present in reproductive tissues and cells of embryonic origin such as the endometrium and trophoblasts, respectively. (PMCID: PMC7511676 PMID: 32353856)
Inorganic iodide and/or iodine is required for optimal cellular function in reproductive tissues, and that iodide transporters may potentially be used as a marker for infertility or for probing potential localized iodine deficiency that may not present in a typical thyroid panel analysis.
- National Health and Nutrition Examination Survey studies show that a significant number of women in childbearing age do not have optimal levels of iodine.
- The need for iodine is not limited to the thyroid glands but its modulatory effects and transporters can be observed in a variety of cells.
- Women with reproductive failures had a significant increase of iodide transporters suggesting a localized iodine deficiency.
Iodine is an essential element that cannot be manufactured in the body and must be obtained through dietary means to ensure adequate metabolic functions. Body organs, including the thyroid, concentrate iodine against a gradient and require adequate iodine levels to produce the necessary thyroid hormones. The World Health Organization (WHO) estimates that almost 2 billion people worldwide do not receive sufficient amounts of iodine.
Localized iodine deficiency could be present in tissues such as the endometrium and may contribute to infertility or reproductive failures by affecting the local immune response and/or regulation of gene expression in reproductive tissues. Given that transporters of iodide have been found in endometrial tissue, it is considered that similar to leukocytes and trophoblastic cells, iodine could affect the functional activity of cells in reproductive tissues including the endometrium. There is no question that iodine deficiency in some women with recurrent reproductive failures is occurring. Iodine is an essential component needed for a successful healthy pregnancy.
The requirement for iodine during pregnancy is substantially increased, by >50%, for multiple reasons. First there is an increased demand for T4 production as it is needed by the fetus in the first trimester. This fetal requirement along with hormonal changes in pregnancy causes alteration in the mother’s thyroid hormone homeostasis and subsequent increased maternal T4 synthesis (30–100% more than pre-pregnancy levels). Second, the fetus utilizes iodine in later trimesters in order to make fetal thyroid hormones. Third, pregnant women have increased iodine clearance/loss. Alteration of thyroid hormone levels due to iodine deficiencies can lead to fetal neurological damage, congenital hypothyroidism, miscarriages, and eventual reproductive failures. Worldwide analysis by the WHO illustrates that iodine deficiencies are prevalent and that includes women in childbearing age. Although organically bound iodine in the form of hormones is essential, iodides and molecular iodine could also play a part in optimizing reproductive organs and pregnancy.
Can Iodine be used while a woman is pregnant?
In Japan, the average Japanese woman is eating 13.8 mg of iodine per day while the average American woman consumes 100 times less iodine per day (approximately 0.138 mg per day). Iodine is very crucial in the first three years of life from the development of the fetus inside the womb until two years after birth. In the development of a child’s IQ, I feel that it would be very advantageous for the mother to supplement her diet during pregnancy and, if she is nursing the child, for the first two years after pregnancy. Pregnant women are notoriously iodine deficient. This data was uncovered in the mainstream press recently. The impact on low birth weight and the baby’s IQ is evident in women with even slight iodine deficiencies.
When breastfeeding, evolution has programmed the mother’s dietary iodine to reroute the lion’s share of her iodine toward nourishing the baby. But the baby still may not get enough from breastfeeding if the mother’s intake is low. Unfortunately, moms rely on prenatal vitamins which usually contain inadequate iodine.
I’ve heard that Iodine prevents breast cancer. Is this true?
We’ve seen a 30 fold increase in breast diseases in the last 50 years. Research does suggest that some breast cancers are linked to an iodine deficiency. It is a fact that as iodine consumption has gone down, breast cancer rates have gone up. It’s interesting to note that Japanese women consume 25X more dietary iodine than American women and have lower breast cancer rates.
Iodine has been determined to actually alter breast cancer-associated gene expressions. It turns off cancer-promoting genes and turns on genes that promote cancer cell apoptosis or cellular destruction. (http://www.medsci.org/v05p0189)
Another study proves that large iodine intake does not adversely affect thyroid hormone production or quality. The researchers did this to allay concerns in the medical profession about potential downsides for using iodine against breast cancer. Iodine, a well-known topical antiseptic and antimicrobial agent, also directly kills cancer cells and serves as the key player in our body’s surveillance system for removing abnormal pre-cancer cells. There is considerable medical research to support this statement. Dr. B.A. Eskin published 80 papers over 30 years researching iodine and breast cancer, and he reports that iodine deficiency causes breast cancer and thyroid cancer in humans and animals. Iodine deficiency is also known to cause a pre-cancerous condition called fibrocystic breast disease. Iodine supplementation which not only resolves breast cysts and fibrocystic breast disease, it also resolves ovarian cysts and thyroid cysts.
Can Iodine help with Breast Tenderness and/or Pain?
Often, when a woman has breast pain, she will be frightened and fear the worst. Thankfully, in most cases breast pain is benign and not a reason to panic. One study showed that breast pain alone is a symptom in only seven percent of women who had early-stage breast cancer, and another eight percent presented with both pain and a lump.1 That said, if you are concerned, see your health care provider.
Breast pain is caused by the fluctuation of fluids. During your menstrual cycle, there is a build-up of fluid in your uterus and your breasts due to inflammatory hormonal changes. When you get your period, some of this fluid leaves your body (when you menstruate). However, the fluid in other parts of your body, like in your breasts, has to be reabsorbed before it can be eliminated.
If you no longer menstruate, it’s still possible for inflammatory hormonal changes to affect your body. This could occur if you eat inflammatory foods, like highly-processed, chemical-laden, or high-glycemic foods. It also occurs when you’re under chronic stress for prolonged periods.
Daily iodine intake can help many women with breast pain. Research shows that those who take iodine in doses ranging from 6 mg to 90 mg per day feel healthier and have a greater sense of well-being. Taking iodine at these levels eliminates breast pain from fibrocystic changes about 70 percent of the time. In one recent study of women with breast pain, more than half of those who took 6 mg of iodine daily reported a significant reduction in overall breast pain.
Iodine decreases the ability of estrogen to adhere to estrogen receptors in the breast. This ties into the compelling evidence that iodine deficiency is a cause of breast cancer. The ductal cells of the breasts, those most likely to become cancerous, actually have an iodine pump in them, indicating that they have the ability to actively absorb iodine. Iodine taken in doses 100 times the RDA (which is only 100–150 mcg per day) has important benefits.
These include its role as an antioxidant, in preventing and treating fibrocystic disease of the breast, and in preventing and treating breast cancer.
I have suggested iodine supplements for women with breast pain and saw excellent results, usually within only two weeks. I recommend a minimum of 12.5 mg/day to start and may have to build up to 50mg daily.
HCG (HUMAN CHORIONIC GONADOTROPIN) HORMONE
HCG is the key hormone detected in positive pregnancy test and can be measured in the urine just 10 days after fertilization. It raises rapidly and peaks at about 10 weeks. It does much more than just “confirm” pregnancy. (remember: LMP means ‘last menstrual period”). Your doctor will monitor this in the beginning of your first trimester to ensure everything is developing as it should be.
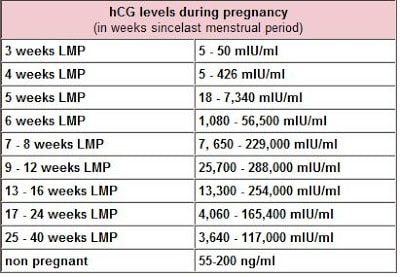
HCG ensures the maintenance of the corpus luteum, a crucial structure that forms in the ovary at the site where a follicle releases an egg during ovulation. During the first 12 weeks, it produces progesterone and estrogens while the placenta is forming. After 12 weeks the placenta takes over hormone production.
HUMAN CHORIONIC SOMATOMAMMOTROPIN (HCS)
This hormone (also known as: human placental lactogen) is a hormone produced by the placenta during pregnancy. It is structurally like human growth hormone and plays several key roles, including regulating maternal metabolism to ensure sufficient glucose and fatty acids for the developing baby and promoting both fetus and placental growth.
PROGESTERONE
Progesterone acts as a key hormone that supports various stages of fetal development and mom’s health too! The word PROGESTERONE literally means FOR GESTATION!
It prepares the uterine lining for implantation of the fertilized egg and maintains this lining throughout the pregnancy. It also prevents the uterus from contracting prematurely. And if you want to know why your boobs grow in the beginning of this journey… blame progesterone… it’s preparing you for breastfeeding!!!
This is another key hormone your doctor should monitor during the first trimester.
Two nutrients that have clinically proven to increase progesterone: Vitamin C and B6 P5P.
If a woman has had low progesterone levels, prior miscarriages, etc. it’s not unusual to have her take more progesterone the first 12 weeks to assist the corpus luteum’s natural production of progesterone. It can be given either topically or orally and even vaginally. Working with a natural doctor to help you manage and monitor is crucial to a successful pregnancy.
ESTROGENS
Estrogen also aids in developing the placenta, is crucial for nutrient and waste exchange between mother and baby and prepares the breast for lactation. Estrogen also contributes to fetal organ development, modulates the mom’s immune system to protect the pregnancy and prepares the body for childbirth by enhancing uterine sensitivity to contractions.
PROLACTIN
This hormone is primarily involved with milk production, but also influences metabolism and fat storage.
INSULIN
During pregnancy, insulin sensitivity greatly decreases mainly due to the two hormones made by the placenta: progesterone and HCS. When insulin sensitivity decreases the mother’s pancreas is stimulation to increase insulin production to help maintain normal blood glucose levels. If the pancreas can keep up with the changes, insulin resistance worsens and GESTATIONAL DIABETES can develop.
RELAXIN
This hormone is primarily produced by the ovaries and the placenta. It loosens and widens the pelvic area’s ligaments and joints, facilitating the necessary expansion for the baby to pass through the birth canal. Relaxin helps to soften and ripen the cervix which is necessary for dilation during the birth process. Some women may have been told that this hormone causes pelvic girdle pain or joint instability during pregnancy but this has been shown to NOT be the case.
To RECAP…
Overall you will notice numerous physiological changes as your body adapts to creating a whole new human being inside of itself. The placenta developing, cardiovascular system works a bit harder, your respiratory system has an increased oxygen consumption of up to 30%, hormonal shifts will be occurring throughout the 9 months, postural changes take place as pregnancy shifts the center of gravity and weakens your abdominal muscles, your pelvic floor and core are both compromised making core rehabilitation and pelvic floor strengthening essential after delivery. Whew! That’s a lot of changes happening in a short period of time. Personally, I don’t think there is a man alive who could get through it with as much grace as we all do!
PREGNANCY “SYMPTOMS & CONSIDERATIONS”
In that first trimester you will certainly experience a number of challenging “symptoms”. Some women might breeze through it …. Another might become totally sidelined by all the symptoms:
Increased heart rate
Headaches
Shortness of breath
Insomnia
Fatigue
Extreme nausea and vomiting
Breast tenderness
Vulva itching
Varicose veins
Leg cramps
Back pain
Dizzy and feeling lightheaded
Frequent urination
It’s like, “DAMN, who’s idea was all this?”
Trust me, if this is your first or even if your other pregnancies went smoothly, these symptoms could kick you in the butt! The fatigue is not like any fatigue you’ve ever experienced. The nausea and vomiting can be overwhelming.
NAUSEA
Let’s take a longer look at the dreaded “nausea & vomiting” symptoms. Nausea and vomiting affect up to 85% of all pregnant women and can greatly impact your and your baby’s nutritional status and mental well-being. Getting up in the middle of the night, heaving and losing the little dinner you got down is stressful to you and your baby.
Typically, the nausea hits you between the 6 to 8 week mark and usually stops before 20 weeks. Rarely, it can last the entire pregnancy. Symptoms can range from persistent nausea to aversion to certain foods or smells, dry heaving, and vomiting all culminating in dehydration and electrolyte imbalances.
The most extreme manifestation of nausea and vomiting that happens to a small percentage of women (less than 10%) is called “hyperemesis gravidarum” (HG) and can lead to critical health issues such as dehydration and metabolic problems which include weight loss, electrolyte imbalances and malnutrition. All of which are harmful to both mother and child. This can lead to a vitamin K deficiency which increases the risk of blood clotting issues. And it’s associated with a range of severe complications, such as brain damage due to lack of B1 thiamine, failure of liver and kidneys, tearing of the esophagus, collapsed lung, high blood pressure, etc. Not a situation to take lightly. If this is occurring and not getting better fast, it’s imperative that you seek medical assistance.
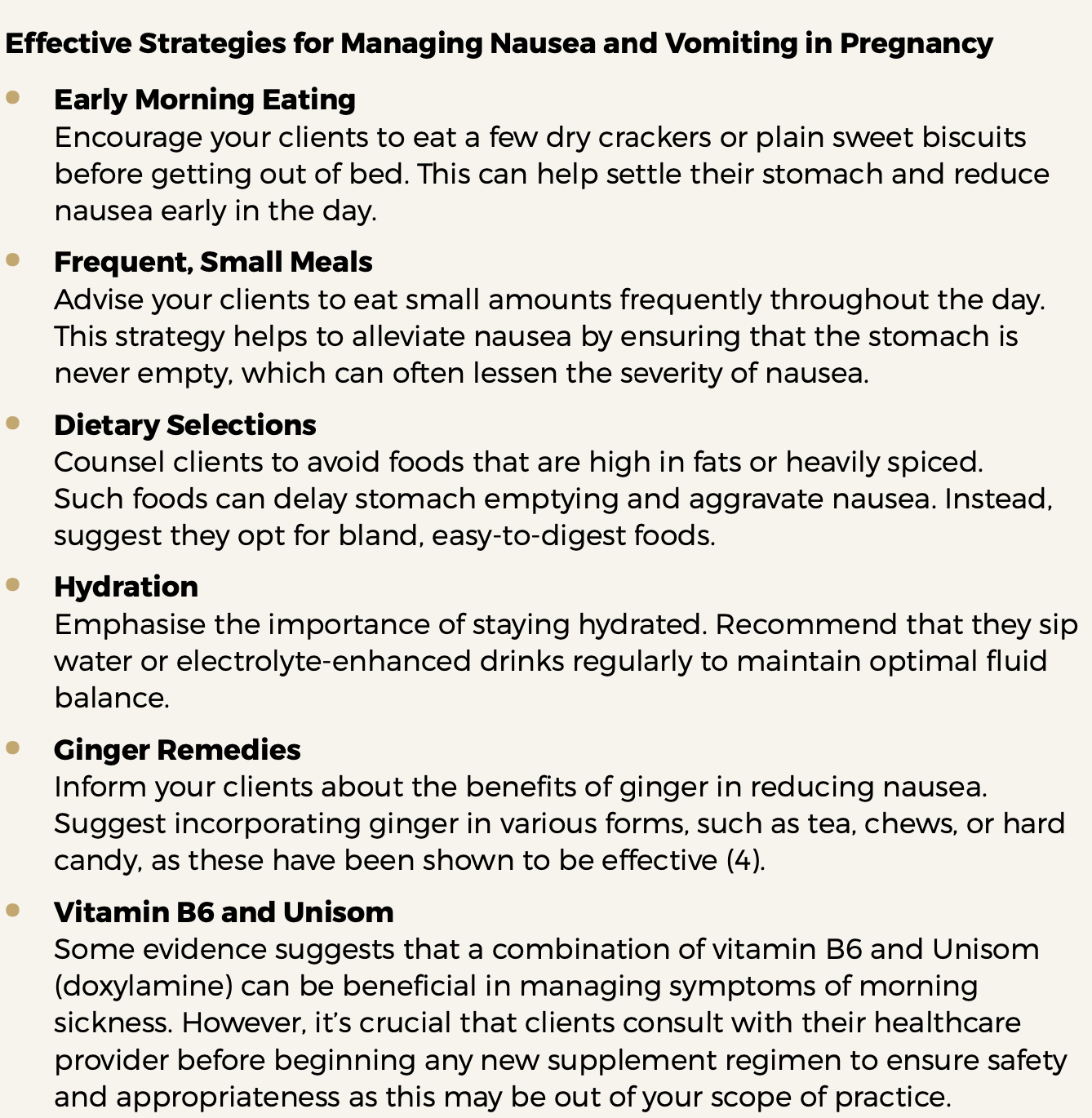
The chart below will give you a few strategies for managing your nausea. The key is in the dosage and consistency to get each strategy to work for you. No two women are the same as to what they need.
If your nausea is nagging but mild, ginger is the first thing to go to. We suggest ginger capsules 500mg each and take 2 each meal and maybe 2 in the afternoon. (We carry in office)
Two interesting studies investigated how vitamin B6 affect people with mild to moderate nausea symptoms. In one study taking B6 60mg of P5P form 3x daily had significant improvements in their nausea symptoms. (Our ASSIST product is a fabulous combination of B6p5p + magnesium and we keep this is stock. )
Taking the over the counter UNISOM (doxylamine) antihistamine has also been shown to help by blocking histamine receptors in the brain and altering neurotransmitter levels which can help reduce nausea symptoms.
Using both B6 p5p and Unisom together would be the last resort. Studies are mixed on the results, but it can be beneficial for some when dealing with moderate to severe nausea.
Another unique way to relieve nausea is smelling isopropyl alcohol. We all know that DRINKING alcohol is a no-no especially during pregnancy but… smelling it can actually help to relieve mild to moderate temporary nausea.
Two trials with about 200 adults found inhaled (smelling) isopropyl alcohol improved mild to moderate nausea and vomiting. For example, after 30 minutes the nausea score improved from 50 out of 100 to 20 with inhaled isopropyl alcohol versus 40 with oral ondansetron!
Patients inhaled deeply as frequently as required to achieve nausea relief from commercially available isopropyl alcohol pads held 1 to 2 cm below the nose. Bottom line: nasally inhaled isopropyl alcohol achieves increased nausea relief compared with placebo during a 10-minute period.
Lindblad AJ, Ting R, Harris K. Inhaled isopropyl alcohol for nausea and vomiting in the emergency department. Can Fam Physician. 2018 Aug;64(8):580. PMID: 30108075; PMCID: PMC6189884.
As a last resort, if natural remedies are not working, there are pharmaceutical interventions available like ondansetron and metoclopramide which can be prescribed by your medical doctor. Yes, they have side effects. But if using them short term helps you to get your nutrition in and stop the stress to your body then it might be the most beneficial thing to take. Sometimes you have to weigh the pros and the cons for you and the baby.
In your second trimester (weeks 13-26) you might begin to feel better than you’ve ever felt. Here comes a surge of energy, negative symptoms start to disappear. This is the best time to start really upping your exercise routines, focus on nutrition, and mentally staying in a safe place.
It’s not unusual to still have breast changes occurring, maybe a little nasal congestion or even a few nosebleeds and varicose veins showing up more pronounced, a little indigestion. This will also be the time you start to feel your baby moving around. An amazing feeling… making it all VERY real: YOU ARE CARRYING A LITTLE HUMAN INSIDE OF YOU!
Then we finally get to the last leg of the race… the third trimester (weeks 27 – BIRTH)
This is the hardest. You’re starting to wear out, back pain may increase. You might notice an increase in shortness of breath due to the growing uterus putting pressure on the diaphragm. That same pressure headed downward can increase urination. In the last few weeks, you might notice intermittent uterine contractions that become intense (called Braxton Hick Contractions). Looking at your feet or hands, you might notice swelling from increased fluid retention. Your sleep might become restless and uncomfortable (you’ve got a baby sitting on and in you!). Fatigue sets in. And finally, anxiety about labor and delivery kicks in. Whew… It’s been a long 9+ months, and then here we are… about to change everything.
What YOU Do Has Generational Effects
“During pregnancy, some baby cells migrate into the mother’s bloodstream and then return to the child. It’s called “fetal microchimerism”. This process involves the transfer of fetal cells into maternal tissues during pregnancy.
For 41 weeks, the FETAL cells migrate into the maternal circulation during pregnancy and can persist in maternal tissues for decades, integrating into various organs such as the bone marrow and other tissues.
Every other child a mother will soon have will leave a similar imprint on her body. Each pregnancy can result in fetal microchimerism, with fetal cells from each offspring potentially persisting in the mother’s body.
Even if a pregnancy doesn’t end, or if you have an abortion, these cells still migrate into the blood flow. Fetal cells can enter the maternal circulation early in pregnancy, and their presence has been detected even in cases of miscarriage or abortion.
Research has shown that if a mother’s heart is injured, fetal cells will rush to the site of the injury, and turn into different types of cells specialized in heart repair.
The child helps the mother repair, while the mother builds the child. And this is possibly the reason why some diseases fade away during pregnancy.
It’s amazing how the mother’s body protects the baby at all costs, and the baby protects and rebuilds the mother in return, so they can safely develop and survive.
Studies have also shown the presence of fetus cells in her mother’s brain 18 years after birth!
How amazing is this?
DIET DURING PREGNANCY
A brand new study found that pregnant women consuming primarily a standard American diet (high fat and processed sugar) increase their risk of birthing a child with ADHD by a startling 66%.
A high-fat, high-sugar Western diet can increase methylation of the IGF2 gene. Methyl groups attach to DNA, acting like an “off switch” that can silence the gene, disrupting fetal brain development in critical areas like the cerebellum and hippocampus.
Diets lacking essential components like omega-3 fatty acids can impair fetal brain development. These fatty acids are crucial for building healthy cell membranes in the brain.
Ultra-processed foods found in the Standard American Diet also expose women to heavy metals. These can accumulate and negatively impact the child’s ability to metabolize and excrete them, influencing the severity of neurodevelopmental disorders like ADHD.
Certain metabolites linked to the Western diet, such as those from high fat and processed sugar intake, promote inflammation and oxidative stress. These factors are known to be critical during early neurodevelopment and contribute to neurodevelopmental disorders.
The early stages of fetal development are particularly sensitive to a mother’s diet. Adopting a balanced, nutrient-rich diet during pregnancy help support brain and organ development, reducing the risk of neurodevelopmental disorders like ADHD. PMID: 33685413
Also, Getting enough protein in daily while avoiding foods that are high risk for bacteria is essential but can be overwhelming for many young moms.
Your body and your immune system are in a different state than normal. This doesn’t mean that you’ve weakened your immune system, but it does involve physiological changes that can increase your susceptibility to certain infections. This heightens your risk to foodborne illnesses such as listeriosis, toxoplasmosis and salmonella.
LIST OF FOODS THAT POSE HIGHER RISKS:
COLD CURED PROCESSED MEATS
DAIRY ITEMS LIKE SOFT CHEESES
PATE’S
RAW SHELLFISH/SEAFOOD
RAW UNDERCOOKED PORK & CHICKEN
RAW EGGS
UNPASTEURISED DAIRY
UNWASHED RAW VEGETABLES, FRUITS, GRAINS
SUSHI – MERCURY CONTAMINATED SEAFOOD
Not all seafood is high in mercury. There are a number of very healthy seafoods that also contain selenium that should be eaten at least weekly. Selenium has a high affinity for mercury, forming a complex with mercury atoms called a selenide compound. This bonding can reduce the bioavailability of mercury and potentially lowering its toxicity. So go enjoy at least weekly the following: Cod, tuna (safe catch), sardines, halibut, shrimp, wild caught salmon, and haddock. (side note: selenium is anti-viral and supports thyroid function!)
Studies consistently highlight the benefits of regular fish consumption during pregnancy due to improvements in a child’s IQ, communication skills and cognitive abilities.

Cross contamination in your own kitchen is also a risk area. Make sure you clean and handwash EVERYTHING especially when handling raw meats, poultry, seafood, eggs and fresh produce. Sanitize utensils, cutting boards, countertops and wash hands liberally.
Keep food separate. Raw meats should be kept away from ready-to-eat foods to prevent bacteria transfer. Even keep meats and seafood in separate grocery bags when shopping.
Cook food thoroughly! Ensure the appropriate internal temp is reached (use a thermometer) to kill off any possible harmful bacteria.
Refrigerate food immediately. Don’t leave out on the counter. Ensure your refrigerator is set below 40 and freeze food below 0-degrees.
ALCOHOL
I hate to break it to you but alcohol before, during and after is never beneficial. During pregnancy specifically, it can cause growth problems, stillbirth, and fetal alcohol spectrum disorder (physical abnormalities, developmental delays, cognitive impairments). And lastly alcohol contributes to cancer.
CAFFEINE
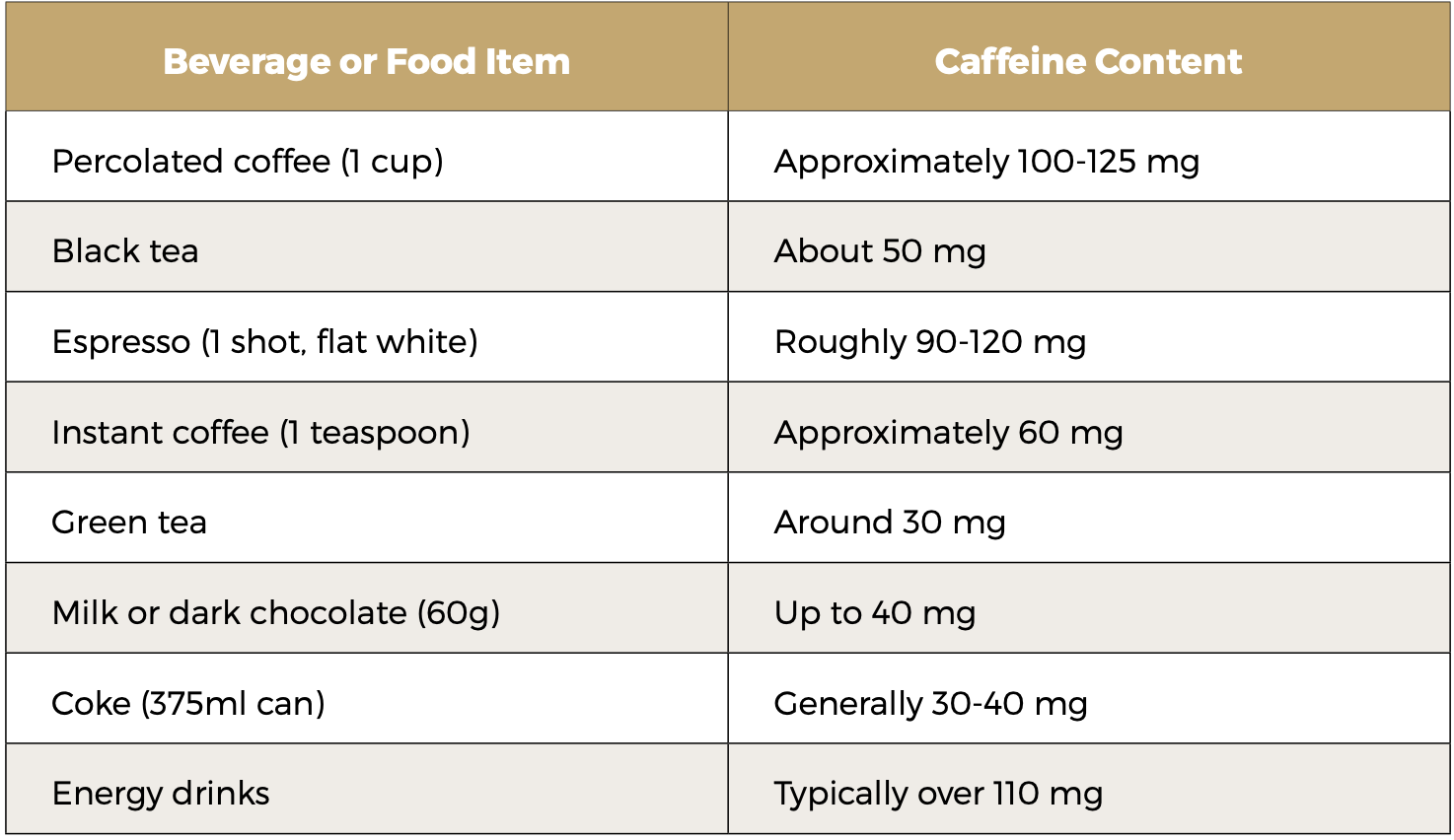
During pregnancy, caffeine passes through the placenta, causing the fetus to be exposed to levels comparable to those in the mother’s system! Studies are inconclusive on the effects. There have been small studies with confounding factors that make it difficult to clearly determine the causes of their outcomes. What has been clear is several studies showing a correlation between elevated caffeine consumption and early miscarriage as well as still birth. The most notable findings pertain to the increased risk of delivering babies with low birth weight in moms with high caffeine intake. Low to moderate caffeine intake (less than 200mg per day) does NOT increase the risk of miscarriage or premature birth. The poison is in the dosage. So, enjoy 1-2 eight ounce cups per day. (each 8 ounce cup of Joe contains approximately 95 mg of caffeine). But make sure you’re also counting the caffeine in your teas, cokes, chocolates and energy drinks as well.
GESTATIONAL DIABETES
Gestational diabetes is a form of diabetes that develops during pregnancy usually in the 3rd trimester. When your body cannot efficiently process glucose due to insulin resistance this resistance stresses the pancreas’ ability to produce sufficient insulin. This is why we counsel our clients to handle their insulin resistance PRIOR TO CONCEPTION if at all possible.
For the mother… gestational diabetes heightens the risk of developing pre-eclampsia, type 2 diabetes, metabolic syndrome, and coronary heart disease and can complicate childbirth. For the baby, it increases the risk of higher birth weights, premature birth, respiratory issues and long-term risk of developing type 2 diabetes. As a mom… be mindful of what you do to your own body and how it will affect your child and their future health. Motherhood starts at conception!!!
A systemic review found that exercise can reduce the risk of gestational diabetes by 38%. This is HUGE. You HAVE to exercise: walk, lift weights, do yoga, do all the things, etc!
Check your blood sugar for a few days. At least do a simple 1 hour glucose challenge test. Go to any drug store and get a little finger prick at-home tester. Drink a 50g glucose solution or simply eat a high glucose food and measure your glucose after 1 hour. If levels are below the thresholds of 130-140 you’re good. If it is consistently higher than that, then do a 3 hour test.
On a 3 hour test you do not fast but eat a balanced first morning meal that is a high protein, low carb breakfast. Wait 3 hours and check your levels again. If consistently higher than 130-140 let your doctor know.
PROTEIN
Most women in general do not consume enough protein whether pregnant or not. But certainly, pregnancy brings its own demands on the body. The most recent research indicates that the protein requirements for healthy pregnant women are significantly higher than previously thought.
The bottom line: get a MINIMUM amount of protein intake 1.5-1.9 grams per kilogram of body weight. Example in pounds: 130 pound woman = 58.967 kg would equate to 112gr of protein daily or 37+ per meal!
Make sure your source of protein is high quality. Plant proteins are good but do have a lower anabolic potential compared to animal proteins but can still support muscle building if consumed in higher quantities. Ensure you read our article on DIETARY GUIDELINES FOR HEALTH for a full rundown on what to eat.
FATS
The recommended total fat intake is 25-30% of total daily energy intake. For a woman who consumes in pregnancy 2060 calories per day, this means she should consume 500-600 calories from fat. Fat typically has about 9 calories per gram to help you figure out how much to eat.
The type of fat is also important. Potato chips, cracklins, seed oils etc. may not be the best. Trans fats should be completely avoided. Track your saturated fat intake. Be honest with yourself and measure and count everything: oils in cooking, nuts snacked on, fat content on processed foods, etc.
You don’t know what you don’t measure!
Do make sure you are taking a high-quality omega 3 supplement. Over the past 50 years or so the intake of omega-3 fatty acids has decreased with an increase in omega-6 fatty acids. The main dietary source of omega 3 is fish. Omega-6 fatty acids are mainly found in sunflower, grapeseed and corn oils along with poultry fats.
In humans we know that omega-3 fatty acids have been found to reduce the risk of pre-eclampsia, lower placenta weight, boost a child’s cognitive development and support linear growth. We’re kind of omega 3 snobs and we’ve made sure that the manufacturer we work with provides for us a very high quality one that is third party tested, guaranteed potency and no heavy metals. So, whether you use ours or another brand, just make sure of the quality.
CARBOHYDRATES
Oh my…. So much debate and hate on carbs! Let’s try to sort through the noise and make some sense of how to handle “CARBS” in your diet.
The human fetus relies on glucose for about 80% of its energy needs, with mom’s glucose crucial for growth and brain development. Glucose moves across the placenta. The recommended carbohydrate intake should be at least 175g per day (58.33 per meal) during pregnancy.
Unrefined carbohydrates that are non starchy offer numerous health benefits as they are rich in micronutrients and fiber. Reducing too much can impair mom’s energy levels and impair fetal growth and cause mom to go into ketosis which is not healthy while pregnant.
Some good examples are: All Sprouts, Artichoke, Asparagus, Broccoli, Celery, Ginger, all leafy Greens, All lettuce, Cucumber, Brussels Sprouts, Onions, Garlic, Bell Peppers, Mushrooms, Radish, Tomatoes, Cabbage, Cauliflower, Zucchini.
Let’s reiterate the key food groups that you need to put emphasis on throughout your pregnancy:
Vegetables: especially cruciferous, like broccoli and cauliflower and green, leafy vegetables, such as spinach and kale
Fruits: a variety of fruits to provide a broad spectrum of vitamins and antioxidants
Eggs: rich in protein and essential nutrients if you can tolerate and are not allergic to them
Salmon and other fatty fish: excellent sources of omega-3 fatty acids crucial for brain development. The only negative is typically high mercury, so keep to once or twice a week and supplement with a good omega three fatty acid like our MAINTAIN supplement.
Quality meats: lean cuts of meat that are high in protein and iron
Nuts & seeds: great for healthy fats and fiber.
VITAMINS – MINERALS – MICRONUTRIENTS
Minerals and vitamins are essential for the health and development of a fetus. Ideally, you should get them from whole foods sources, but our earth and our foods are sadly not as rich and bountiful in nutrients as they used to be. For that reason you’ll most likely need a good prenatal vitamin along with the other key nutrients not easily available incorrect form through whole foods sources only.
SUPPLEMENTS YOU MIGHT NEED:
Now that you’ve got your main food groups from whole foods sources, let’s take a look at a few key supplements that you might need.
A good high quality prenatal vitamin is essential. Just because a supplement is called “prenatal” doesn’t mean that it’s good for you. Work with your practitioner to make sure you’re getting the highest quality, not just those that are highly promoted on social media. We spoke earlier about the importance of iodine (not just any iodine will help – work with a practitioner who can guide you correctly). Vitamin D3 ( which is technically a pro-hormone) is also essential and we want this at the upper level of its range. Before supplementing with vitamin D3, it should be checked in serum tests.
Vitamin C
Vitamin C is important for both mom and baby’s health during pregnancy. It plays an essential role in the synthesis of collagen, important for the baby’s developing skin, tendons, bones, and cartilage. Additionally, it supports the mothers immune system, helping toward off infections. You also need vitamin C to help your body absorb the iron that you intake. There’s also evidence to suggest that vitamin C is vital for fetal brain development. You should get at least 85mg of vitamin C daily, which is a very small amount and very easy to get through your diet… if you’re eating fruits and vegetables like oranges strawberries, bell peppers, broccoli, you’re gonna be just fine. The minimum is 85 mg but one study recently found that consuming more than 200 mg of vitamins per day from dietary sources, not supplements, such as fruits and vegetables, can significantly lower the risk of developing gestational diabetes!
Vitamin B 12
B12(the methylated form) is crucial during pregnancy as it supports vital functions essential for both the mother’s health and fetal development. It plays a key role in the proper formation of the nervous system of the fetus, including the neural tube, and the deficiency can lead to neural tube defects, such as spina bifida. Vitamin B12 is also critical to produce red blood cells, helping to prevent anemia. Additionally, it’s involved in the DNA synthesis and cell replication processes that are especially important during pregnancy due to rapid cell division. It aids in the metabolism of proteins, fats, and carbohydrates.
FOLATE
Folate intake before and during pregnancy is crucial to prevent neural tube defects and other congenital malformations in the baby. These kind of defects occur in the first few weeks of pregnancy often before a woman even know she’s pregnant. So if a woman is trying to conceive I immediately start them on a good folate supplement with the proper form of B vitamins.
Folate is essential for cell division, gene regulation, amino acid metabolism, and neurotransmitter synthesis. During pregnancy more folate is needed for the rapid growth of the uterus, placenta fetus and maternal blood volume. Pregnant women require 5 to 10 times more folate than non-pregnant women putting them at risk for deficiency.
Foods high in natural folate are: spinach, asparagus, Brussels sprouts, broccoli, avocado, lentils, black beans, peas, romaine, lettuce, oranges, beef, liver, eggs.
FOLATE VS FOLIC ACID
Folic acid and folate are closely related but not identical. Folate is a natural form of vitamin B9 found in foods. Folic acid is the synthetic version used in supplements in fortified foods. Since the neural tube closes within the first four weeks of pregnancy, often before a woman realizes she has even pregnant, maintaining adequate folate levels or taking folate supplements before conception is essential. We always use in our pre and post natal protocols the methylated form of folate to ensure proper absorption and utilization.
CHOLINE
The benefits of Choline have not been known for as long as those of folate and research on choline is relatively newer. As a result, the importance of choline is not always communicated to the general public.
Choline is the vital nutrient for both mothers and their developing babies. It’s a water soluble compound necessary for building cell membranes and producing acetylcholine, a neurotransmitter that is important for brain function. It’s also vital for liver function and during pregnancy can help prevent neural tube defects, enhance cognitive development of the baby and support the mother‘s health. Supplementation can fill the gap when dietary intake is not sufficient. Supplementing with 250 to 350 a day is ideal during pregnancy or eat plenty of choline rich foods weekly.
Food high in choline: eggs, beef, liver, chicken liver, salmon, cooked soy beans, Brussels sprouts, broccoli.
Vitamin D3, Iodine and iron area all necessary to ensure both you and your baby are healthy. Work with your natural practitioner to check and monitor these levels at the beginning of your pregnancy, mid pregnancy and again right after delivery!
Vitamin D3, Iodine and iron area all necessary to ensure both you and your baby are healthy. Work with your natural practitioner to check and monitor these levels at the beginning of your pregnancy, mid pregnancy and again right after delivery!
I’ll cover more on this topic when we discuss POSTNATAL protocols.
EXERCISE
Movement during pregnancy is vital. I hear of so many doctors suggesting for their pregnant clients/patients to ‘not lift anything heavy’. This is just factually stupid. Think about the mother with three kids. I can guarantee you…. She was hauling around one kid 50 pounds or more in one arm while dragging another behind her and a purse on her shoulder! I heard one doctor suggest to their patient to not bend over! What the heck are they thinking? What do you think their own Mother did when they were pregnant with them? It boggles the mind.
Exercise and movement is vital. And I’m not talking about just cardiovascular. I’m talking about doing heavy resistance training that can even be done while pregnant. At this time, I don’t know of any well done randomized control trial that examines the safety of heavy resistance training during pregnancy. But I do know hundreds of women who are pregnant, had children while pregnant, picked up heavy grocery bags, moved furniture, picked up children squirming & crying and fighting back, etc.. I would call that resistance training.
But due to the lack of high-quality evidence guidelines have always tended to be very conservative. Pregnancy is naturally a very protective time in a woman’s life and recommendations do err on the side of caution… Even though more and more women are participating in sports and challenging the notion they should be sedentary or reduce their training loads as soon as they become pregnant.
If you want to do yoga, weightlifting, running, etc. go for it. Make sure you monitor your health. Ideally have a trainer or somebody to spot for you but whatever you do, don’t stop moving. We know for a fact that being active during pregnancy can lower the chance of having gestational diabetes by 38%, preeclampsia by 41%, gestational hypertension by 39%, and prenatal depression by 67%! It also decreases the chance of having a very large baby by 39%.
Even if you come into your pregnancy with complications and health issues physically there’s always something that you can do to move your body, even if it’s walking and holding 3 pound weights, working with bands, yoga, etc.
BASIC EXERCISE GUIDELINES
*Doing any physical activity is better than doing none. If you’re currently doing no physical activity start by doing some and gradually build up to the recommended amount.
*Be active on most, preferably all, days every week.
*Accumulate 2 1/2 to 5 hours of moderate intensity physical activity or 11/4 to 2 1/2 hours of vigorous physical activity or an equivalent combination of both moderate and vigorous activities, each week.
*Do muscle strengthening activities on at least two days each week.
*Minimize the amount of time spent in prolonged sitting.
*Break up long periods of sitting as often as possible.
Do you make sure that you don’t overwork yourself. If you experience, chest pain, shortness of breath, severe headaches, persistent dizziness, painful uterine contractions, vaginal bleeding, or continuous loss of fluid from the vagina make sure you seek medical help right away.
Our STANDARD PROTOCOL (pre- and post- natal)
As a holistic practitioner, I am well aware that all supplements are not created equally. After doing personal trials with many labs I chose to work with a few of the top ones producing supplements that I know are safe, of the highest quality, with clean ingredients, & are tested for potency, purity and performance. These labs have also assisted me in the development of my own supplement brand. All of our supplements are gluten and dairy free, all B vitamins are methylated, and all are manufactured following Good Manufacturing Practices (GMP). Please note that other nutrients might also be needed, but what is listed below is non-negotiable …
Foundation Multi vitamin : 1 in am 1 pm
Active B complex with methylfolate : 1 in am
Assist B6 P5P + magnesium : 2 in pm
Immunity D3 1 in pm per testing
Emotion progesterone as needed by testing
Maintain omega 3 : 1 in am 1 in pm
Vital Aminos 1 scoop in water or smoothie daily
Daily elements micro greens 1- 2 scoops in water or smoothie (provides whole food sources for vitamin C, K, zinc, choline, etc. & minerals) Use this link below to order yours today: https://getdailyelements.com/thatshealth for 15% off 1st purchase use code: MARIEPACE
All supplements are available on our website with full info on each to educate you thoroughly. https://thatshealth.com/shop/
NOTE ON PROGESTERONE: if you were taking progesterone and finally achieved a positive pregnancy test, you MUST STAY on progesterone for the entire 1st trimester (no matter what you’re ObGyn tells you!). Depending on your individual needs we might suggest increasing for the 1st trimester or even adding in vaginal use. It is very individualized based on your history and current status.
POST-NATAL
HOW TO HANDLE POST-NATAL HEALTH
Whew! You did it. You and your baby made it through 9 months of wild physical and emotional changes and you both made it through the delivery…
NOW WHAT?
Ok, you are now VERY aware that your entire body has changed. Every muscle and every cell has altered. It’s now time to get your body back in to shape… but hold on there, wild woman… not too fast! Let have you do a gradual progression of exercise intensity.. up to 150 minutes of moderate to vigorous physical activity such as:
Begin each day with 10-15 minutes up to 30 minutes of vigorous walking or body weight exercises. At 6 -8 weeks you can add in resistance. Start slow and build gently with gradual wight increases.
Work on strengthening the pelvic floor with pelvic tilts, Kegels and move up to planks and hip bridges. Walk every day. Cycle after 6 weeks, swim after 8 and running after 12 weeks. Moving too fast through these stages can cause harm to your body. So move but don’t push it.
If you’re breastfeeding, we suggest do that BEFORE you exercise each day. Ensure you are getting adequate hydration and nutrition and wear a good sports bra to help you maintain a strong milk supply.
If you have any heavy bleeding, pain or persistent pelvic floor heaviness or pain you must not start exercising until those issues are resolved. If there are any postpartum pre-eclampsia symptoms, you should also refrain from exercise until resolved.
URINARY INCONTINENCE
Urinary incontinence (UI), which is the involuntary loss of urine, affects a significant number of women. Its prevalence is estimated to be between 25% and 45% in the general female population. However, this rate can be much higher in certain sports. For instance, around 80% of women in high-impact sports like trampolining report UI, compared to 5.56% to 25.9% in non-impact activities such as yoga and Pilates.
Risk Factors for UI
- Age
- High Body Mass Index (BMI)
- Vaginal Childbirth – Women 2.4 times more likely to have UI than a caesarean birth (29)
- Strenuous exercise specifically in adolescent athletes (30)
- Chronic Coughing
Incontinence is not limited to pregnant or postpartum women. In fact, many athletic women also experience incontinence. The reasons why young female athletes who haven’t had children experience more urinary incontinence (UI) than those who are not active are still unclear. Some ideas suggest that it might be due to factors like pelvic floor movement during activities like jumping and running, fatigue of pelvic floor muscles from intense exercise, and changes in the pelvic floor muscles. Additionally, low energy levels, low body mass index (BMI), changes in estrogen, and joint hypermobility might also contribute to UI in female athletes.
POSTPARTUM NUTRITION
Proper energy and nutrient intake during lactation is critical. It prevents nutritional deficiencies in the mother, supports a healthy return to pre-pregnancy weight, and influences the composition of breast milk, which is essential for the infant’s development.
Sadly medical doctors (OBGYNs and pediatricians) are not trained at all in nutrition and exercise and literally none mention anything until after the 6 week check up (too little too late). Unfortunately, many breastfeeding women don’t meet the recommended intake for energy and nutrients, which complicates nutritional interventions!
Postpartum nutrition is crucial for recovery, breastfeeding, and overall well-being. It focuses on supporting the mother’s physical healing, energy levels, and milk production if breastfeeding.
Key considerations include:
- Energy Requirements
- Macronutrient Requirements
- Micronutrient Requirements Hydration
Postpartum women face significant barriers to managing their weight and lifestyle and consuming a high-quality diet, making them more vulnerable and at higher risk in our increasingly obesogenic environment. Some of these barriers include:
Women experience significant changes in sleep, life challenges, and stress after giving birth. An adult’s sleep cycle differs significantly from a newborn. While adults experience 90-minute sleep cycles consisting of multiple stages (light, deep, and REM sleep) and usually sleep in a consolidated period at night, newborns have shorter 20 to 50-minute sleep cycles. Newborns spend more time in REM sleep, essential for brain development, and their sleep is divided into short bursts throughout the day and night due to frequent feeding needs.
Additionally, newborns often enter REM sleep soon after falling asleep and lack mature circadian rhythms, which develop over the first few months of life. This means that your client will face extreme fluctuations in their sleep patterns, which are not always limited to the newborn phase.
Many mothers continue to experience sleep challenges for years after their babies are born.
Postpartum women are also more likely to experience depressive symptoms during this period. Poor sleep, high stress, and depression are linked to weight gain in the general population. Sleeping less than 5 hours is not uncommon for postpartum women and can contribute to weigh gain and obesity due to becoming insulin resistant with this lack of sleep.
It’s also pretty darn hard to keep a schedule with a newborn. Between lack of sleep, trying to breastfeed, work, grocery shopping, cleaning the house, trying to exercise daily, taking care of their other babies (ie. Other kids and/or Husband!), sustaining all these changes and eating healthy becomes quite the challenge. Every day will be something new. Learning to juggle all of this and maintain your own health will be crucial and at times difficult. There might need to be some give and take in each area as you juggle it all.
What’s most important is YOUR NUTRITION. What you eat or don’t eat affects not just you but your child. During both pregnancy and during lactation women’s nutritional needs increase compared to when they are not pregnant. Some of these nutrients are needed in much higher quantities when breastfeeding.
|
Core food group |
Breast- feeding (serves per day) |
Not breast- feeding (serves per day) |
Examples of one standard serve |
|
Vegetables and legumes/beans |
7.5 |
5 |
|
|
Fruit |
2 |
2 |
• 30 g dried fruit (such as 4 apricot halves, 11⁄2 tablespoons sultanas) |
|
Grain (cereal) foods, mostly wholegrain and/or high-fibre varieties |
9 |
6 |
|
|
Core food group |
Breast- feeding (serves per day) |
Not breast- feeding (serves per day) |
Examples of one standard serve |
|
Lean meats and poultry, fish, eggs, tofu, nuts and seeds, and legumes/ beans |
2.5 |
2.5 |
• 65 g cooked lean meats, such as beef, lamb, veal, pork • (90–100 g raw) • 80 g cooked lean poultry, such as chicken, turkey (100 g raw) • 100 g cooked fish fillet (115 g raw) or 1 small can of fish • 2 large eggs • 1 cup cooked or canned legumes/beans, such as lentils or chickpeas • 30 g nuts or seeds |
|
Milk, yoghurt, cheese and/ |
2.5 |
2.5 |
• 1 cup (250 ml) fresh, long-life or reconstituted powdered milk • 2 slices (40 g) hard cheese, such as cheddar • % cup (200 g) yoghurt • 1 cup (250 mL) soy, rice or other cereal drink, with >100 mg calcium per 100 mL |
This chart is a good example of core food groups and servings for women age 19-50
KEY NUTRIENTS
IODINE – Iodine plays a critical role in producing thyroid hormones (T4 and T3), which are essential for infant growth and brain development. If your client’s iodine intake is insufficient, she risks becoming deficient, which could also affect her baby. Breastfed infants rely on breastmilk for their iodine intake, making it important for breastfeeding mothers to meet their iodine needs. Women at higher risk of deficiency include those who smoke, avoid dairy or seafood, do not use iodised salt, or regularly consume goitrogen-rich foods like kale, cabbage, or broccoli. We suggest for all breastfeeding women to consume our IODORAL supplement both prenatally and during breastfeeding for their babies’ health.
IRON INTAKE – Iron is a crucial mineral needed for various body functions, including the production of red blood cells, oxygen transport, energy generation, immune support, and oxygen storage in muscles. Postpartum women require sufficient iron to recover from childbirth and prevent deficiency. Symptoms of iron deficiency can include fatigue, weakness, pale skin, and shortness of breath. Dietary iron comes in two forms: haem iron from animal sources, which is easily absorbed, and non-haem iron from plant sources, which is less efficiently absorbed.
During postpartum recovery, women may be at risk of iron deficiency due to increased needs, blood loss, and dietary challenges.
During pregnancy, iron needs increase to 27 mg per day but then drop to 9 mg per day for breastfeeding women. Interestingly, the recommended iron intake for non-pregnant, non-lactating women is 18 mg per day, which is double the recommendation for breastfeeding women. The reason for this difference is that breastfeeding suppresses the hormones responsible for ovulation, often leading to amenorrhea (the absence of periods).
Suckling stimulates a brain pathway that increases prolactin, which supports milk production while also suppressing ovulation. As a result, many women do not menstruate until they reduce breastfeeding or stop altogether.
The lower iron recommendation for breastfeeding women is based on the assumption that they are not ovulating and therefore not losing blood through menstruation. However, once menstruation returns, iron needs should increase back to pre-pregnancy levels of 18 mg per day. If your client is breastfeeding and her period returns, her iron needs will rise accordingly. It’s important to note that women who breastfeed and have their menstruation return might experience more irregular periods compared to those who aren’t breastfeeding. Given this,
I recommend basing their iron intake on the 18 mg per day guideline when menstruation resumes.
I strongly recommend that all postpartum women undergo a blood panel to check for nutrient deficiencies, particularly iron and vitamin D levels. If iron deficiency anemia is diagnosed, supplementation may be required, typically taking 6-12 months to restore optimal levels. High-dose iron supplements (100-200mg) are often necessary, but some women may experience constipation, which can strain the pelvic floor. I suggest options like Pro-Ferrin brand being gentler on the digestive system, especially for those prone to constipation.
If you find yourself having the “Baby Blues”, don’t panic. We can help you. If you’re breastfeeding it is a little more difficult as we usually like to see you get back onto progesterone. But while breastfeeding we don’t suggest hormones! But what you can do is our custom ASSIST product at 2 each meal ALONG with our MOOD supplement.
If you have any issues, just give us a call. Don’t allow yourself to stay “down”. We are here to help you.
Breastfeeding
Special note: I you choose to have IV fluids at birth and or need them, newborn weight and loss/gain can account for this in the first weeks.
In 2011 a team of Canadian researchers published a study which linked routine IV fluids with excessive weight loss in newborns. The study concluded that it takes about 24 hours for babies to correct their fluid state and therefore a true birth weight should be done at 24 hours. Here’s the issue with with weighing baby at birth with a mother who received IV fluids: those fluids not only over saturate the mother (throwing her into an electrolyte imbalance), but this same thing happens to baby!
HOW TO INCREASE MILK SUPPLY
It is quite possible that some herbal remedies will help increase milk supply and flow of milk to the baby. Almost every culture has some sort of herb, plant, or natural source potion to increase milk supply. Some may work, some may work as placebos (which is fine), and some may not work at all. Some will have active ingredients that will not increase the milk supply but have other effects, which may not be desirable. If a drug, even herbal and natural, has a positive effect, it can also have negative effects. For example, foxglove, a commonly grown flower, contains digitalis which has been used to treat heart failure. But ingest too much foxglove and it can cause serious side effects and even death.
To emphasize, note that even herbs can have side effects, even serious ones. Natural source drugs are still drugs, and there is no such thing as a 100% safe drug. Luckily, as with most drugs, the baby will get only a tiny percentage of the mother’s dose, which means the baby is extremely unlikely to have any side effects.
If you take other medications or supplements or have any health conditions, check with your doctor or pharmacist before starting any of the remedies below.
Fenugreek and Blessed Thistle
Fenugreek: 3 capsules 3 times a day Blessed Thistle: 3 capsules 3 times a day, or 20 drops of the tincture 3 times a day
Fenugreek and blessed thistle seem to work better if you take both, not just one or the other. Note that there is no good proof that they really work at all.
These herbs work quickly. If they do work, and you will usually notice a difference within 24 hours of starting them. If there is no effect by 72 hours, they probably will not work.
Fenugreek is sometimes sold as a combination with thyme. Do not buy this combination.
Herbal remedies are not standardized. You may see bottles of fenugreek and blessed thistle with the number of milligrams in each capsule listed but nobody really know how much of the active ingredient is in each capsule.
Use 3 capsules of each herb 3 times a day as a starting point.
Shatavari
Powder: 2 teaspoons stirred into warm milk 1 to 2 times per day. This is the traditional ayurvedic formulation for the powdered root. It can probably be mixed with other beverages if you do not consume dairy.
Capsules: 1 to 2 500 mg capsules, 2 times per day
Shatavari comes from the same family as asparagus.
It is traditionally used in China and India for various conditions, including infertility and increasing milk production.
Other herbal treatments that have been used, but may or may not work to increase milk supply are:
Alfalfa
Fennel seed
Red raspberry leaf
Stinging nettle
Food that may help increase milk supply:
Oatmeal
Garlic, in moderation
Ginger, in moderation
Many cultures have traditional foods they have found helpful (fish and papaya soup, hot curry dishes, etc.).
Herbs to be avoided while breastfeeding
This list has been compiled from numerous authoritative sources, however, it may not be complete and individuals should always err on the side of caution.
- Aloe vera latex (not juice) (Aloe spp.)
- Black cohosh (Actaea racemosa)
- Bladderwrack (Fucus vesiculosus)
- Blue cohosh (Caulophyllum thalictroides)
- Borage (Borago officinalis)
- Buckthorn fruit (Rhamnus cathartica)
- Bugleweed leaf (Lycopus spp)
- Cinchona bark (Cinchona spp)
- Cola seeds (Cola nitida)*
- Coltsfoot leaf (Tussilago farfara)
- Comfrey leaf/root (Symphytum officinale)
- Ephedra (Ephedra spp.)
- Uva Ursi
- Thyme
- Kava Kava
- Dong Quai
- Ginseng
- Guarana (Paullinia cupana)*
- Rhodiola
- Jasmine flowers (Jasminum pubescens)
- Kava (Piper methysticum)
- Madder root (Rubia tinctorum)
- Ma Huang (Ephedra sinica)
- Pulsatilla (Anemone pulsatilla)
- Queen of the Meadow root/herb (Eupatorium purpureum)
- Senecio (Senecio aureus)
- Wormwood herb (Artemesia absinthium)
Safe Supplements post natal and during breast feeding (in most cases, work with your natural practitioner to determine what’s good for you):
Gaba in lower amounts
Lavendar
DHA fatty acid
L-Theanine
Phosphatidylserine
B vitamins and D3
Saffron
______________________
Ok. So we’ve discussed nutrition and action for both mom and dad pre- and post- natal. But what about your new baby? What do they need?
For a newborn, especially a breastfed baby, vitamin D supplementation is crucial. Babies need 400 IU (10 mcg) of vitamin D daily, starting soon after birth, until they are weaned or drink at least 32 ounces of formula with vitamin D. Infant formula is fortified with vitamin D, so formula-fed babies only need a supplement if they consume less than 32 ounces daily. Additionally, iron supplementation is recommended for breastfed babies around 4 months of age. We strongly encourage new mom’s to have on hand before delivery so they can start immediately giving 400iu minimally to their baby right at birth.
A good probiotic should also be used. We do carry in our office an excellent blend. Our infant formula is a gentle probiotic blend containing 10 carefully selected species, specifically selected to help support the gut health of infants and young children.
This formula is particularly beneficial for babies who have experienced cesarean birth, formula feeding, exposure to medications, environmental stressors, or changes in the maternal diet. It can easily be mixed with breast milk, formula or food and is perfect from birth to 3 years of age. This product is made without common allergens, including milk/casein, eggs, fish, shellfish, tree nuts, peanuts, wheat, gluten, soybeans, and sesame.
REFERENCES:
-
Roberts, B. M., Nuckols, G., & Krieger, J. W. (2020). Sex Differences in Resistance Training: A Systematic Review and Meta-Analysis. Journal of strength and conditioning research, 34(5), 1448–1460. https://doi.org/10.1519/JSC.0000000000003521
-
Tagawa R, Watanabe D, Ito K, Ueda K, Nakayama K, Sanbongi C, Miyachi M. Dose- response relationship between protein intake and muscle mass increase: a systematic review and meta-analysis of randomized controlled trials. Nutr Rev. 2020 Nov 4;79(1):66–75. doi: 10.1093/nutrit/nuaa104. Epub ahead of print. PMID: 33300582; PMCID: PMC7727026.
-
Wycherley TP, Moran LJ, Clifton PM, Noakes M, Brinkworth GD. Effects of energy- restricted high-protein, low-fat compared with standard-protein, low-fat diets: a meta- analysis of randomized controlled trials. Am J Clin Nutr. 2012 Dec;96(6):1281-98. doi: 10.3945/ajcn.112.044321. Epub 2012 Oct 24. PMID: 23097268.
-
Li P, Yin YL, Li D, Kim SW, Wu G. Amino acids and immune function. Br J Nutr. 2007 Aug;98(2):237-52. doi: 10.1017/S000711450769936X. Epub 2007 Apr 3. PMID: 17403271.
-
Cruzat VF, Krause M, Newsholme P. Amino acid supplementation and impact on immune function in the context of exercise. J Int Soc Sports Nutr. 2014 Dec 14;11(1):61. doi: 10.1186/s12970-014-0061-8. PMID: 25530736; PMCID: PMC4272512.
-
Hodges RE, Minich DM. Modulation of Metabolic Detoxification Pathways Using Foods and Food-Derived Components: A Scientific Review with Clinical Application. J Nutr Metab. 2015;2015:760689. doi:10.1155/2015/760689
-
Feinman RD, Fine EJ. “A calorie is a calorie” violates the second law of thermodynamics. Nutr J. 2004 Jul 28;3:9.
-
Veldhorst M, Smeets A, Soenen S, Hochstenbach-Waelen A, Hursel R, Diepvens K, Lejeune M, Luscombe-Marsh N, Westerterp-Plantenga M. Protein-induced satiety: effects and mechanisms of different proteins. Physiol Behav. 2008 May 23;94(2):300-7. doi: 10.1016/j.physbeh.2008.01.003. Epub 2008 Jan 12. PMID: 18282589.
-
Wolf, R. Skeletal muscle protein metabolism and resistance exercise. Journal of Nutrition. 2006; 136(2):525S-528S
-
Surampudi P, Enkhmaa B, Anuurad E, Berglund L. Lipid Lowering with Soluble Dietary Fiber. Curr Atheroscler Rep. 2016 Dec;18(12):75. doi: 10.1007/s11883-016-0624-z. PMID: 27807734.
-
Makki K, Deehan EC, Walter J, Bäckhed F. The Impact of Dietary Fiber on Gut Microbiota in Host Health and Disease. Cell Host Microbe. 2018 Jun 13;23(6):705-715. doi: 10.1016/j.chom.2018.05.012. PMID: 29902436.
-
Anderson JW, Baird P, Davis RH Jr, Ferreri S, Knudtson M, Koraym A, Waters V, Williams CL. Health benefits of dietary fiber. Nutr Rev. 2009 Apr;67(4):188-205. doi: 10.1111/j.1753- 4887.2009.00189.x. PMID: 19335713.
-
-
Refalo, M.C., Helms, E.R., Trexler, E.T. et al. Influence of Resistance Training Proximity- to-Failure on Skeletal Muscle Hypertrophy: A Systematic Review with Meta- analysis. Sports Med 53, 649–665 (2023). https://doi.org/10.1007/s40279-022-01784-y
-
Schoenfeld BJ, Grgic J, Ogborn D, Krieger JW. Strength and Hypertrophy Adaptations Between Low- vs. High-Load Resistance Training: A Systematic Review and Meta-analysis. J Strength Cond Res. 2017 Dec;31(12):3508-3523. doi: 10.1519/ JSC.0000000000002200. PMID: 28834797.
-
Baz-Valle E, Balsalobre-Fernández C, Alix-Fages C, Santos-Concejero J. A Systematic Review of The Effects of Different Resistance Training Volumes on Muscle Hypertrophy. J Hum Kinet. 2022 Feb 10;81:199-210. doi: 10.2478/hukin-2022-0017. PMID: 35291645; PMCID: PMC8884877.
-
Grgic J, Schoenfeld BJ, Davies TB, Lazinica B, Krieger JW, Pedisic Z. Effect of Resistance Training Frequency on Gains in Muscular Strength: A Systematic Review and Meta- Analysis. Sports Med. 2018 May;48(5):1207-1220. doi: 10.1007/s40279-018-0872-x. PMID: 29470825.
-
van Vliet S, Beals JW, Holwerda AM, Emmons RS, Goessens JP, Paluska SA, De Lisio M, van Loon LJC, Burd NA. Time-dependent regulation of postprandial muscle protein synthesis rates after milk protein ingestion in young men. J Appl Physiol (1985). 2019 Dec 1;127(6):1792-1801. doi: 10.1152/japplphysiol.00608.2019. Epub 2019 Nov 14. PMID: 31725358; PMCID: PMC7054632.
-
Rhea MR, Alvar BA, Burkett LN, Ball SD. A meta-analysis to determine the dose response for strength development. Med Sci Sports Exerc. Mar 2003;35(3):456-464.
-
https://pubmed.ncbi.nlm.nih.gov/33093862/?utm_source=chatgpt.com
-
https://pmc.ncbi.nlm.nih.gov/articles/PMC4989712/?utm_source=chatgpt.com
-
ttps://touroscholar.touro.edu/cgi/viewcontent.cgi?article=1254&context=sjlcas&utm_source=chatgpt.com
-
Legal: The information provided is not intended as a means of diagnosis or treating illness or as a replacement for any medicine or advice from a competent physician. Individuals having serious health problems should consult a competent licensed physician specializing in their condition. The FDA has not evaluated these statements. We assume no responsibility for anyone choosing to self-administer any suggestions in this publication; they do so on their own determinism. The information in this publication is for educational purposes only.
Copyright 2025. All Rights Reserved. Optimum Solutions LLC dba THAT’S HEALTH